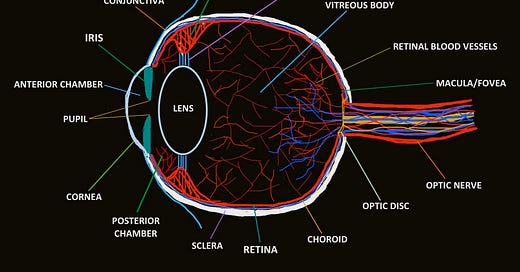
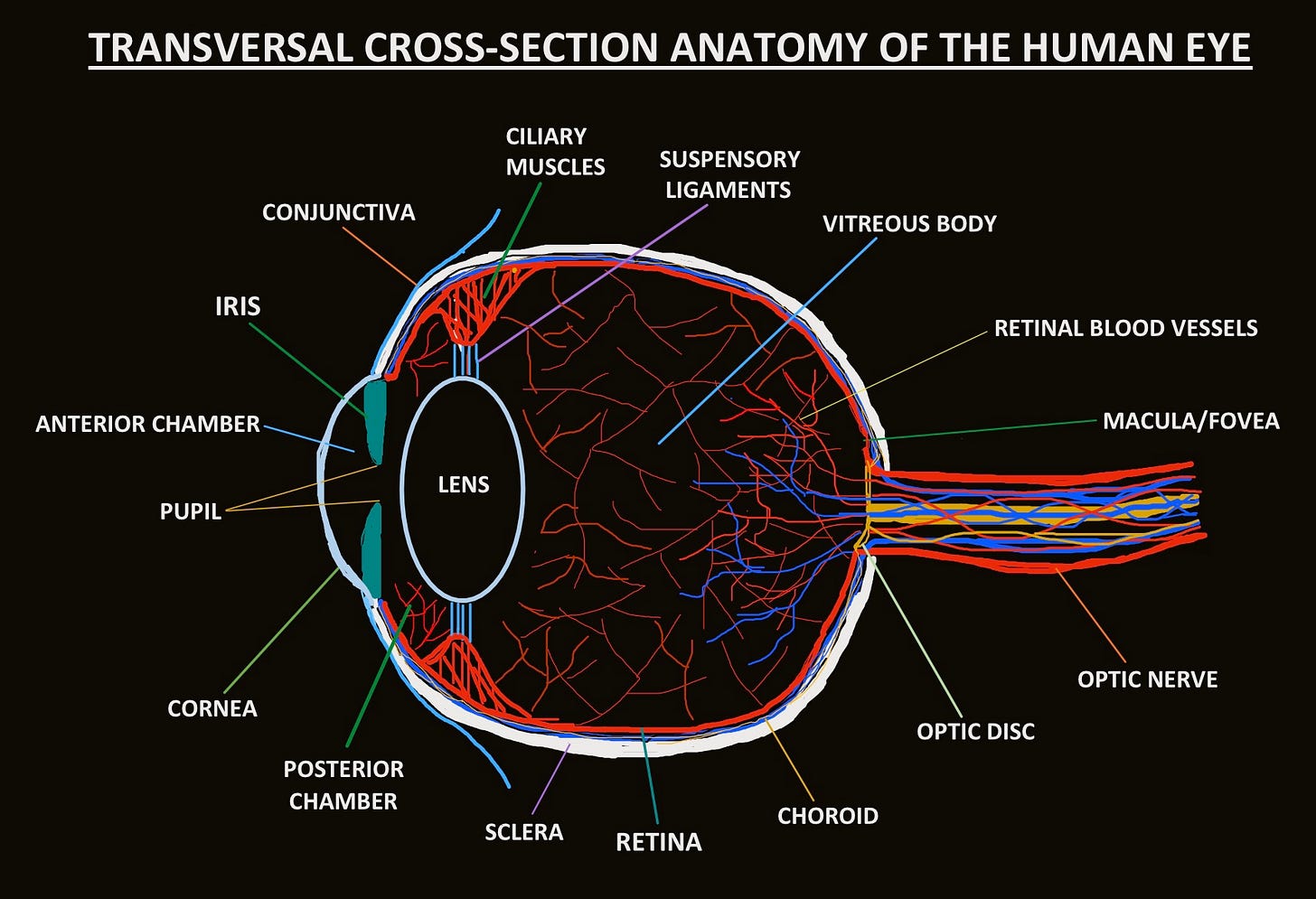
THE THREE LAYERS OF THE HUMAN EYE
SCLERA
The sclera is the opaque, fibrous, outermost layer of the human eye that forms the “white” of the eye. Composed mainly of collagen and some elastic fibre, it forms the protective, supporting barrier of the eyeball and is continuous with the cornea at the anterior of the eye and the dural sheath of the optic nerve at the posterior of the eye. The sclera is mainly made up of type 1 collagen fibres, forming highly dense and rigid connective tissue. The reason that the sclera is white and opaque while the cornea is transparent is that the collagen fibres in the sclera are oriented in different directions while the cornea’s collagen fibres are arranged in a parallel conformation. However, despite their different orientations, the collagen fibres of the sclera and cornea are continuous with each other. The thin, clear conjunctiva covers the anterior part of the sclera (visible to the outside world), and the eye’s seven extraocular muscles connect to the eyeball through the sclera. Despite sometimes being confused with each other, there are some key differences between the conjunctiva and the sclera that must be highlighted. The conjunctiva is a thin, transparent layer of tissue that covers the sclera and lines the eyes and eyelids. It is a functional layer that is heavily involved in maintaining the homeostasis of the tear film and protects the eye from pathogens, staving off potential infections. The sclera, on the other hand, serves a solely structural purpose as it gives the eye rigidity and physical protection. Relative to the other layers of the eye, the sclera is metabolically inactive as it has a very limited blood supply. The entire layer is avascular and receives only a small amount of nutrients from parts of the choroid. It is merely a lifeless collection of collagen fibres that maintains the spherical shape of the eye and protects it from injury.
CHOROID
The choroid is the vascular, central layer of the eye that is sandwiched between the retina and the sclera. It consists of connective tissue that is composed of a dense network of blood vessels (mainly capillaries) that supply oxygen and nutrients to the retinal pigment epithelium (RPE) and the outer nuclear layer of the retina. The choroid’s thickness ranges from 0.1 mm to 0.2 mm, making it the thinnest of the human eye’s three main layers.
The choroid shares the retinal pigment epithelial cells with the retina. Similar to the iris, these cells contain the dark-coloured pigment, melanin, which absorbs and filters natural light to protect the neural layers of the retina and restricts reflections within the eye that could potentially harm vision. The innermost layer of the choroid is known as Bruch’s membrane, a 5-layered structure which, in conjunction with the retinal pigment epithelium, forms a compartment between the retina and the choroid. This is an essential function because any structural defect in either layer can cause the growth of blood vessels from the choroid to the retina or vice versa. The retina is of vital importance in the eye, as its absence would make vision impossible. Thus, without the choroid which constantly supplies the retina with oxygen and nutrients through its dense network of blood vessels, the cells of the retina would die and the retina would cease to function — speaking to the vitality of the choroid in making vision possible.
RETINA
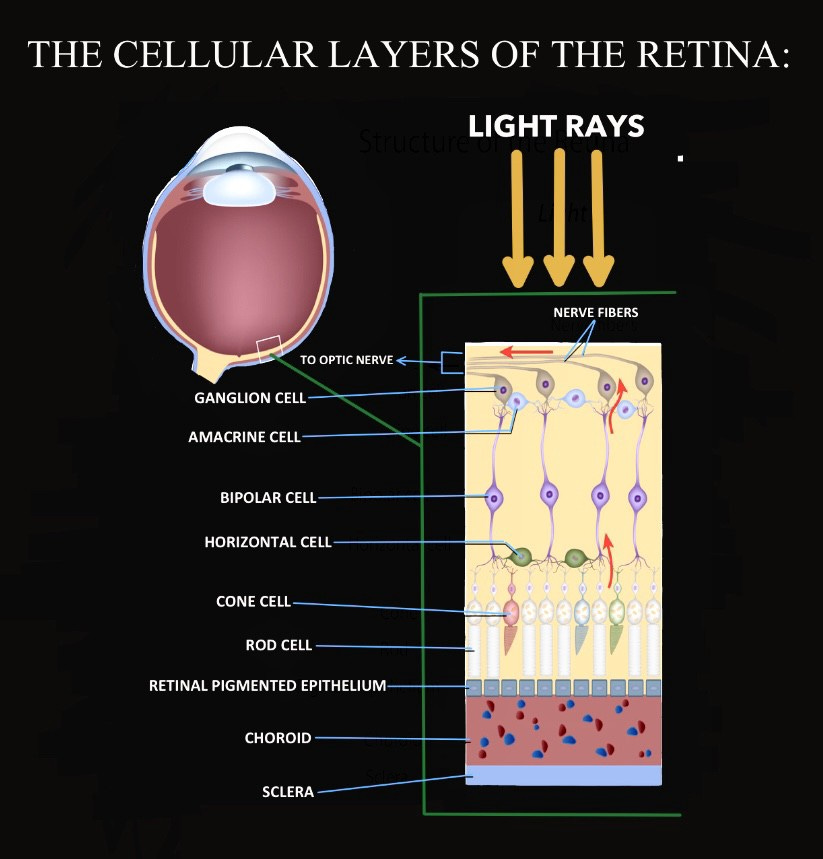
The retina is arguably the most important, yet delicate, part of the eye that enables vision. It’s a thin, light-sensitive layer of tissue that covers approximately 65 percent of the back of the eye. Fundamentally, the retina’s function is to receive light that has been focused onto it by the cornea and the lens, convert it into neural signals through photoreceptors, and transmit these signals to the occipital lobe of the brain via the optic nerve for visual recognition.
The retina consists of photoreceptors called rods and cones. Rods are responsible for detecting low levels of light in dim conditions, while cones are responsible for processing detailed, colour vision. These photoreceptors are spread out all across the retina — except for the porus opticus where the optic nerve pierces the bulb of the eye, in which there are solely retinal ganglion cell axons. The retina consists of a small region near its centre known as the macula that contains the highest concentration of light-sensitive cone cells and is responsible for sharp, central vision.
The photosensitive layer is composed of several cellular layers that work in coalition to convert light into visual information in the form of electrical signals and send these signals to the brain via the optic nerve (as can be seen in figure 3). It all begins in the outer nuclear layer where the nuclei of rods and cones receive light from the surrounding environment and convert the light rays into neural signals that carry visual information. These neural signals then travel through the axons of the rods and cones in the outer plexiform layer to the nuclei of horizontal cells in the inner nuclear layer. From there, the signals travel horizontally toward the bipolar cells and are transmitted via neurotransmitters from the axon terminals of the horizontal cells to the nuclei of bipolar cells. The bipolar cells pick up the neural signals at their dendrites, which then travel across their nerve axons to the amacrine cell. The amacrine cells finally relay the neural signals to the dendrites of ganglion cells which branch in the inner plexiform layer — a particularly important region in the retina that is composed of a dense reticulum of neurofibrils formed by interlaced dendrites of retinal ganglion cells and the cells of the inner nuclear layer, namely horizontal, bipolar, amacrine, and Müller cells (which provide anti-oxidative support for photoreceptors and maintain the intactness of the blood-retinal barrier). After receiving the neural signals at their dendrites, the retinal ganglion cells transmit the signals through their long axons all the way to the visual processing centres in the occipital lobe at the posterior of the brain. The axons of retinal ganglion cells essentially congregate at the optic disc, where they become myelinated and collectively form the optic nerve. Since the visual information is transmitted over a relatively significant distance, it is encoded as strains of action potentials (also known as neural impulses). These neural impulses “jump” from one node of Ranvier — unmyelinated regions in the axonal membrane between Schwann cells — to another, accelerating neural transmission along the optic nerve between the retina and the visual cortex. Out of all structures in the human eye, the retina plays the most complex and crucial role for enabling sight.
Retinal Blood Vessels
The retina is supplied with blood by a dense and delicate network of blood vessels. The retinal blood vessels are basically the central retinal artery (arteria centralis retinæ) and vein (vena centralis retinæ), as well as their accompanying branches. The arteria centralis retinæ and vena centralis retinæ perforate the optic nerve and enter the eye through the optic disc (porus opticus), splitting into the superior (upper) and inferior (lower) branches. The retinal blood vessels provide blood to the inner retinal neurons, which is essential for them to function effectively. Since most of the light entering the eye is focused onto the macula in the central retina, most of the blood that the retina is supplied with through the retinal blood vessels nourishes the macula. Retinal blood vessels can be damaged by diabetes, hypertension (high blood pressure) and other physiological conditions, and are particularly susceptible due to their delicacy. This is just one of the many important reasons to maintain good cardiovascular health. The retinal vasculature is rich and dense, supplying the capillaries that run into and nourish neural tissue. Without them, the retina, and thus vision, would not be able to function.
ANTERIOR SEGMENT STRUCTURES
CONJUNCTIVA
The conjunctiva is the thin, transparent, moist membrane that covers the front of the eye and lines the inside of the eyelids. It lubricates and protects the eye by the secretion of mucus and tears, and also plays a significant role in immunosurveillance by preventing the entry of microbes into the eye. Keeping the inner surface of the eyelids moist and lubricated is important so that they can open and close easily without friction, which could irritate the eye. For the general health of the eye, consistently protecting it from dust, debris and infection-causing pathogens in the environment is also crucial, and this protection can be achieved thanks to the conjunctiva. The inner layer of the conjunctiva coats the inner surfaces of the eyelids and is known as the palpebral conjunctiva, while the outer layer of the conjunctiva which coats the outer surface of the eye is known as ocular, or bulbar, conjunctiva. The most common condition associated with the conjunctiva is conjunctivitis, more colloquially known as “pink eye”, which is inflammation of the lining of the conjunctiva.
CORNEA
The cornea is the thin, convex, transparent layer that covers the anterior chamber, iris, and pupil of the eye. It is a tissue that constitutes no blood vessels — the only one of its kind in the body — and consists of a tear film on its outside which is composed of 3 layers: the mucin layer, the aqueous layer, and the lipid layer. The primary function of the cornea is to refract light coming from outside into the eye through the pupil. Approximately 2/3rds of the eye’s total refractive power comes from the cornea (43 dioptres), however, unlike the lens, it can not change shape for accommodation. The cornea ultimately serves to protect the inside of the eye from particles in the surrounding environment and plays a big role in refracting incoming light rays.
ANTERIOR CHAMBER
The anterior chamber is a cavity located at the anterior part of the eye which occupies the space between the cornea and the iris. The anterior chamber is filled with a fluid called aqueous humour, a transparent fluid that fills the space between the crystalline lens and the cornea. Aqueous humour is produced by the epithelium of the ciliary body, where it is secreted into the posterior chamber and flows into the anterior chamber through the pupil. The fluid is mainly composed of water and is essential for the health of the eye. It nourishes the cornea and lens with nutrition such as amino acids and glucose and also works to ensure the stability of the pressure within the eye, known as intraocular pressure (IOP).
PUPIL
The pupil is the circular opening of the eye through which light enters. It is the contractile aperture at the centre of the iris, the pigmented, adjustable diaphragm of the eye which adjusts the size of the pupil to accommodate different levels of light that enter the eye. Compared to a photographic lens, the pupil is like the opening at the centre of the lens that admits light from the surrounding environment, while the iris of the eye is like the diaphragm of a camera which limits the aperture of the photographic lens.
IRIS

The iris is a pigmented and ring-shaped muscular structure between the cornea and lens which encircles the pupil. It is a thin, fibrous muscle that consists of connective tissue and is primarily composed of two layers; the pigmented fibrovascular layer known as the stroma, and behind that, the pigmented epithelium layer. The iris is basically an adjustable diaphragm that controls the amount of light that enters the eye through the pupil. The iris does this by constricting to decrease the diameter of the pupil in order to allow less light into the eye in a brighter environment, or by dilating to increase the diameter of the pupil in order to allow more light into the eye in a dimmer environment. The iris consists of two smooth muscles that work to achieve these actions: the sphincter muscle, which plays a role in the constriction of the pupil, and the dilator muscle, which plays a role in the dilation of the pupil. The iris is famous for resembling the unique eye colour of an individual. It receives this quality from a biological pigment known as melanin. The more melanin an individual’s iris has, the darker their eye colour, and the less melanin, the lighter their eye colour (blue eyes, for instance). Without the iris, it would be impossible to control the amount of light that enters the eye and this could damage the retina, which is critical in converting the controlled amount of light that it receives from the outside environment into visual information.
POSTERIOR CHAMBER
The posterior chamber is a narrow cavity located behind the peripheral part of the iris and anterior to the suspensory ligaments of the lens and the ciliary processes. It is an important structure involved in the circulation of aqueous humour in the anterior segment of the eye. Specifically, aqueous humour is produced by the epithelium of the ciliary body and is secreted into the posterior chamber, from which it flows through the pupil to enter the anterior chamber. The iris divides the two chambers while the crystalline lens divides the eye into the anterior segment, located anterior to the lens, and the posterior segment, located posterior to the lens.
LENS
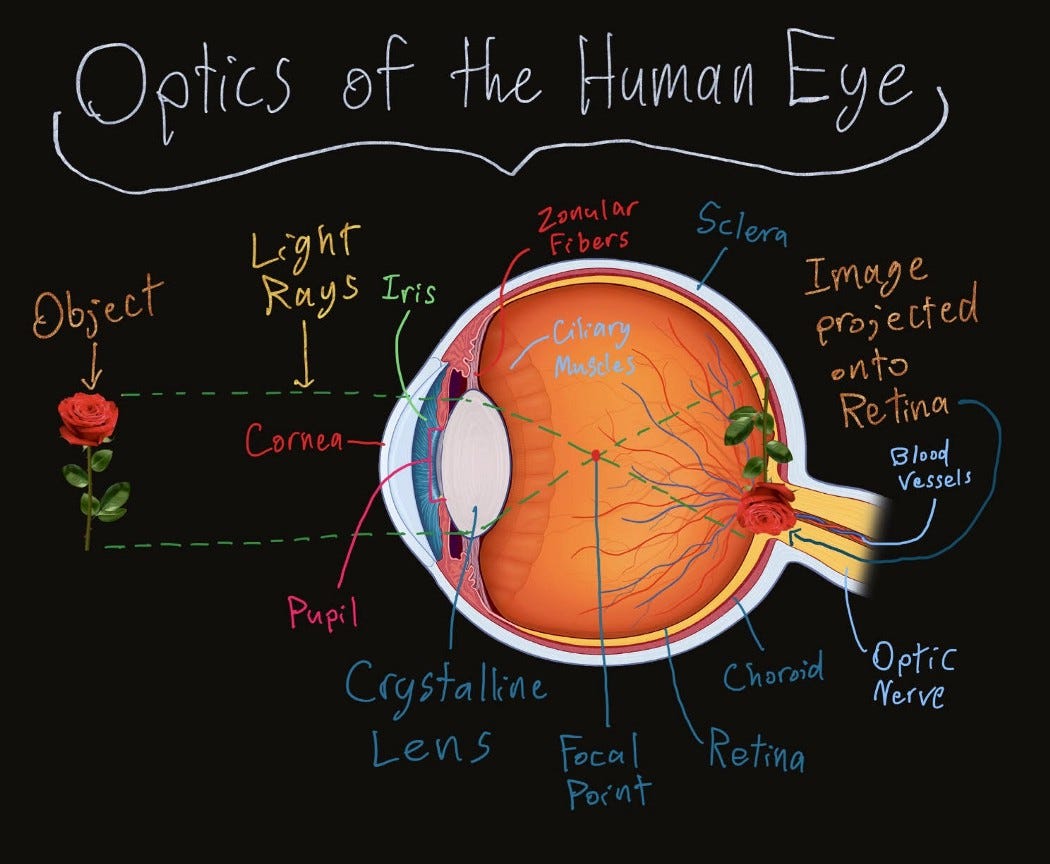
The lens, also known as the crystalline lens, is an important structure in the eye that, along with the cornea, plays a critical role in refracting light from the surrounding environment. It is a transparent, crystalline, biconvex structure located behind the iris and the pupil, perpendicular to the ciliary body. The lens accounts for approximately 1/3 of the eye’s total refracting power (18 dioptres). Unlike the cornea which sustains a static shape, the lens is dynamic as it has the ability to change shape and accommodate to refract light coming from objects at varying distances. The lens is attached to and controlled by the ciliary muscles and suspensory ligaments in the posterior chamber. These two work in conjunction to change the shape of the lens for accommodation and are responsible for making the lens more spherical (increasing refractive power) to accommodate light entering the eye from nearby objects, and flattening the lens (decreasing refractive power) to accommodate light entering the eye from distant objects. The dynamic and flexible crystalline lens of the eye functions to “fine-tune” the light refracted by the cornea and focus it onto the retina to achieve a clear, high-definition image of the surrounding environment.
CILIARY BODY
The ciliary body is part of the eye, located in the posterior chamber, that connects the iris to the choroid (the eye’s blood vessel-rich middle layer, sandwiched between the sclera and the retina). It has three main functions: accommodation of the lens, aqueous humour production and resorption, and maintenance of the lens zonules for the purpose of anchoring the lens in place. The ciliary body consists of the ciliary muscle, a series of radial ciliary processes (from which the lens is suspended by ligaments), and the ciliary ring, which adjoins the choroid. The ciliary muscles are primarily responsible for changing the shape of the lens for accommodation, and they work in coalition with the suspensory ligaments in order to achieve this. The suspensory ligaments connect the lens to the ciliary body. They are made of a collection of zonular fibres, which are connective tissues that anchor the “equator” of the lens and the adjacent anterior and posterior surface of the lens to the ciliary body as well as the ciliary section of the retina. Together, they form the ciliary zonule, a ring of fibrous strands connecting the ciliary body with the crystalline lens of the eye. To make the lens more spherical to accommodate light entering the eye from nearby objects, the ciliary muscles contract, while the suspensory ligaments relax. On the other hand, to flatten the lens to accommodate light entering the eye from distant objects, the ciliary muscles relax, while the suspensory ligaments contract.
POSTERIOR SEGMENT STRUCTURES
VITREOUS BODY
The vitreous body is the clear gel that fills the space between the lens and the retina of the eyeball of humans and other vertebrates. The vitreous body consists of a transparent gelatinous tissue called the vitreous humour. 99% of vitreous humour is composed of water and the remaining 1% is a mixture of collagen, various proteins, salts and sugars. The vitreous humour performs a vital role in protecting the eye as it helps the eye sustain its spherical shape, filling the hollow centre of the eyeball. The vitreous humour also comes in contact with the retina (the tissue at the back of the eye that acts like the film of a camera), keeping the essential light-sensitive layer of the eye from detachment.
MACULA/FOVEA
The macula, also known as the macula lutea, is a small region located near the centre of the retina, the light-sensitive layer of the eye. It is a yellowish, oval-shaped area that surrounds the fovea, also known as the fovea centralis. Together, the macula and fovea form the region of keenest vision in the retina as it gives us the ability to see the quality “20/20” vision and provides the finest colour vision. The fovea is a tiny pit in the retina aligned with the central axis of the lens, whereas the macula is a larger area including and surrounding the fovea. The fovea contains about 4,000 tiny, densely packed cones (no rods, however) and produces the highest visual resolution (also known as visual acuity). It is essentially part of the retina that is responsible for sharp, detailed central vision (also known as foveal vision), which is necessary for tasks such as reading, driving, and any other activity for which visual detail is of high importance. Cones are photoreceptor cells that are responsible for detecting and distinguishing colour and detail. Since the fovea centralis has a very high concentration of cones, this is the reason why it provides the highest visual acuity.
OPTIC DISC
The optic disc, also known as the blind spot of the eye, is a tiny region located at the porus opticus, where the optic nerve connects to the bulb of the eye. The optic disc is known as the blind spot because there are no retinal photoreceptor cells located in the region. Consequently, when light rays enter the eye and come in contact with the optic disc since there are no photoreceptors to convert the light rays into electrical signals for visual processing, a small part of your visual field would be impaired. However, the visual cortex in the occipital lobe of the brain compensates for this blind spot in the visual field. The occipital lobe translates the electrical impulses that it receives from the eye into vision. When it receives visual information from a specific object or place, that information is recorded and saved as visual memory. Therefore, using this visual memory, the brain compensates for what you can’t see due to the blind spot in your visual field.
OPTIC NERVE
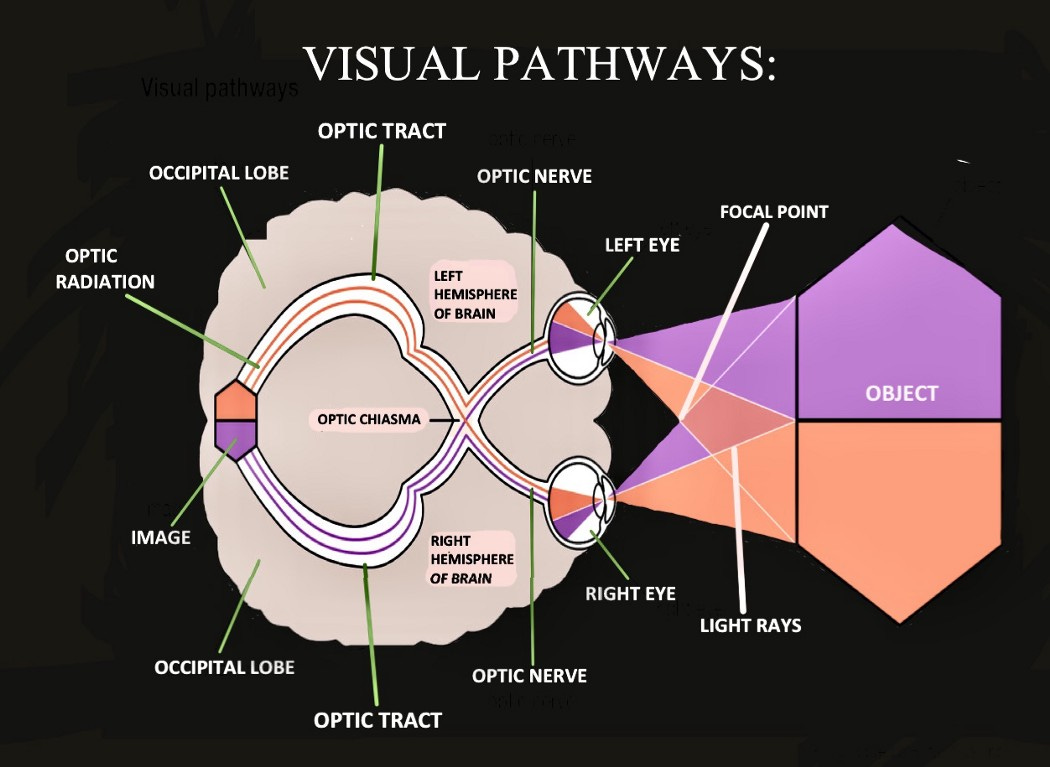
The optic nerve is the main nerve that connects the retina of the eye to the occipital lobe (also known as the visual cortex) located at the rear of the brain. The optic nerve connects to the retina at the optic disc, also known as the blind spot (no photoreceptors are found here). It is the second cranial nerve*, also called cranial nerve II. The main function of the optic nerve is to transmit visual information from the retina of the eye to the vision centres of the brain, located in the occipital lobe, through electrical impulses. These electrical impulses are generated by the photoreceptor cells of the retina and “carry” visual information, which is transferred by the axons of retinal ganglion cells to the visual cortex. In the visual cortex, the information for the flat, two-dimensional images carried by the electrical impulses from the retina is used to construct three-dimensional images to help us visually perceive the environment around us. Specifically, visual features such as colour, line, shape, texture, pattern, tone and size are carefully analyzed and put together to help us develop depth perception and view the world in three dimensions. This entire visual transmission and processing system occurs at a shockingly rapid speed. According to a team of neuroscientists from the Massachusetts Institute of Technology (MIT) in Cambridge, Massachusetts, the human brain is able to process entire images that the eye sees in as little as just 13 milliseconds.
*The cranial nerves are 12 pairs of nerves that connect the brain to different parts of the head, neck, and torso. Each is named after its structure or function and has a corresponding Roman numeral between I and XII. This number is based on their location from the anterior to the posterior section of the head/neck/torso.
Since the image that is projected onto our retinae is originally upside down, the neurons in the occipital lobe “flip” the image right-side up so that we perceive the world in the correct orientation. Each human optic nerve contains between 770,000 and 1.7 million nerve fibres. Specifically, these nerve fibres are the axons of retinal ganglion cells which project out from the inner plexiform layer of the retina. In the fovea, these ganglion cells connect to as few as 5 photoreceptor cells while in other areas of the retina, they connect to thousands of photoreceptors. Although the optic nerve is found in the eye, it is part of the central nervous system (CNS). The optic nerve allows us to make sense of what we are seeing, and without it, even if the eyes are healthy, vision would not be possible.
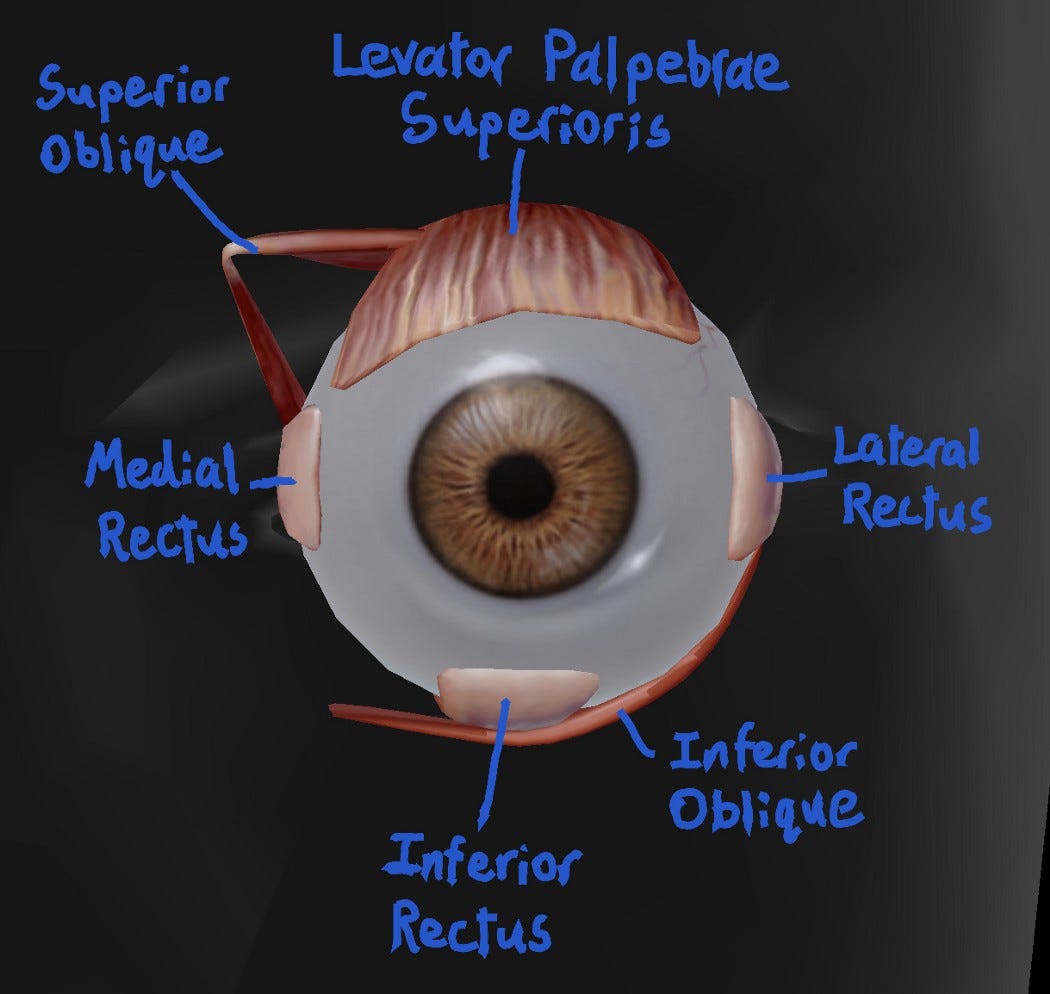
EXTRAOCULAR MUSCLES OF THE EYE
The extraocular muscles are a set of seven muscles surrounding the bulb of each eye that control the eyes’ movements. They each originate at a particular structure posterior to the eyeball and are innervated by one of three cranial nerves (III, IV, or VI). There are four rectus muscles that move the eyes in the four cardinal directions, two oblique muscles that move the eyes inwards and outwards as well the four cardinal directions in conjunction with the rectus muscles, and the levator palpebrae superioris which has the sole function of raising the upper eyelid. Below is an overview of each extraocular muscle outlining its origin, innervation, and function.
Superior Rectus
Origin: annulus of Zinn
Innervation: superior division of the oculomotor nerve (cranial nerve III)
Function: elevation, adduction, and intorsion of the eyeball
Inferior Rectus
Origin: annulus of Zinn
Innervation: inferior division of the oculomotor nerve (cranial nerve III)
Function: depression, adduction, and extortion of the eyeball
Medial Rectus
Origin: annulus of Zinn
Innervation: inferior division of the oculomotor nerve (cranial nerve III)
Function: adduction (medial movement → towards the midline of the body) of the eyeball
Lateral Rectus
Origin: annulus of Zinn
Innervation: abducens nerve (cranial nerve VI)
Function: abduction (lateral movement → away from the body) of the eyeball
Superior Oblique
Origin: sphenoid bone
Innervation: trochlear nerve (cranial nerve IV)
Function: depression, abduction, and intorsion of the eyeball
Inferior Oblique
Origin: maxillary bone
Innervation: inferior division of the oculomotor nerve (cranial nerve III)
Function: elevation, abduction, and extortion of the eyeball
Levator Palpebrae Superioris
Origin: sphenoid bone
Innervation: oculomotor nerve (cranial nerve III)
Function: elevation of the upper eyelid
THE LACRIMAL APPARATUS
The lacrimal apparatus is a complex system of glands, ducts, and tissues responsible for the production, secretion, and drainage of tears. Tears are essential for maintaining the health and function of the eyes as they provide lubrication, nourishment (essential nutrients and oxygen), and protection against pathogens and thus infection thanks to the enzymes and antibodies present inside them. The lacrimal apparatus is composed of several components, each with a specific function that contributes in some way to the unwearied system of tear generation and circulation.
The main components of the lacrimal apparatus include the lacrimal gland, the accessory lacrimal glands, the lacrimal canaliculi, the lacrimal sac, and the nasolacrimal duct. The lacrimal glad, located in the upper outer corner of the eye socket, is the primary producer of tears. The gland is divided into two parts: the orbital and palpebral portions. The orbital portion is responsible for producing basal tears, while the palpebral portion produces reflex tears in response to irritation or emotional stimuli.
The accessory lacrimal glands are small glands located in the conjunctiva, the thin membrane that covers the sclera of the eye and the inner surface of the eyelids. These glands produce small quantities of tears that supplement the larger tears produced by the lacrimal gland.
The lacrimal canaliculi are tiny channels that drain tears from the eye’s surface into the lacrimal sac. There are two canaliculi in each eye, one in the upper eyelid and one in the lower eyelid. The canaliculi are lined with specialized cells called epithelial cells that help propel tears toward the lacrimal sac.
The lacrimal sac is a small, pear-shaped structure located in the lacrimal fossa, a depression in the bone near the nose. The lacrimal sac’s function is to collect tears from the canaliculi and empty them into the nasolacrimal duct.
The nasolacrimal duct is a narrow tube that connects the lacrimal sac to the nasal cavity. The duct begins at the inferior end of the lacrimal sac and passes through a bony canal known as the nasolacrimal duct canal, which opens into the inferior meatus of the nose. Tears that are not absorbed by the eye’s surface flow into the nasolacrimal duct and are eventually drained into the nose and throat. This is why when you cry you tend to develop a runny nose and swallow some salty tears. However, it is all worth it considering the crucial role that the lacrimal apparatus plays in keeping our eyes healthy through the constant production and circulation of tears.